Stepping Up Technology to Improve Health Care
“…Technologies excite me, as they present immense opportunities for the future. Among the many countries in the world, those which prepare for this change and build the foundations to take advantage of such technological advancements will prosper and develop. Those which are not able to do so will invariably be left behind.” His Majesty Jigme Khesar Namgyel Wangchuck.1
The use of Information Communication Technology (ICT) in various facets of governance — around the world and in Bhutan to an extent — has greatly advanced over the years. The application of ICT has shown significant impact in overcoming social, geographical and economic barriers in access to healthcare services. Apart from enhancing access to and delivery of healthcare services, digitisation of services has also resulted in sharper control over monitoring, evaluation and supervisory initiatives.
Bhutan, with a population of more than 0.7 million, is served by more than 5,0002 healthcare professionals, which include doctors, nurses, medical technicians and others, through more than 3002 health facilities. As Bhutan adopts digital initiatives, many programmes in the ministry are projecting the need for electronic systems and mobile applications to collect data and introduce evidence-based decision-making.
The Royal Government of Bhutan has accorded priority to tapping the potential of ICT in various sectors. Guided by the vision, “the nation with the best health”, the health sector has emphasised the importance of using ICT-enabled solutions to improve the delivery of quality care to the people of Bhutan. Clause 5.4 of the National Health Policy of Bhutan, 2011, states that “The Royal Government of Bhutan shall provide 100 percent nationwide access to a health care professional through technology-enabled solutions”. Furthermore, Clause 7.2 of National Health Policy 2011 states that “Digitised Health record and information systems shall be instituted in all the health facilities for faster and effective health information generation to support decision-making.”3
The health sector currently uses around 20 different ICT systems and has 15 ICT professionals spread across the ministry, hospitals, and other offices around the country to support health workers as well as the health facilities and offices. The e-health solutions being used include the District Health Information System version 2 (DHIS2), open source software rolled out in 2014 with the support of WHO, to collect numerous aggregated reports from the field. The same system is also used for tracking Mother and Child Health (MCH), malaria, and other purposes. A National Early Warning, Alert and Response Surveillance (NEWARS) system is used by the Royal Centre for Disease Control under the health ministry for reporting and monitoring disease outbreaks. The Electronic Bhutan Medical Supplies and Inventory System (eBMSIS) has been used by the ministry and health facilities for indentation, procurement, supplies and inventory of medicines and other medical supplies since 2017.
The Blood Transfusion System is used for blood stock inventory and donor management by the blood banks. A Call Centre System is used by the Health Help Centre for emergency management. The K-Tracker is a GIS-based system used for ambulance movement. A Picture Archiving and Communication System (PACS) is used by the national referral hospital for radio image viewing and archiving. A donated proprietary Laboratory Information System (LIS) is used by labs in hospitals for blood test management.
Other smaller systems include DocApp, Water Quality Monitoring Information System, Measles and Rubella Surveillance Information System, Tuberculosis Information and Surveillance System, Influenza-Like Illness and Severe Acute Respiratory Infection System, Bhutan Diarrheal Surveillance Information System, Salt Iodine Monitoring System, Climate Informed Health Early Warning System, and Bhutan Febrile & Malaria Information System.
Some of the external systems the ministry uses centrally are electronic Payments Expenditure Management System, Civil Services Information System, Government Performance Management System and electronic Government Procurement System. Some of these are used very efficiently, while some have become obsolete and redundant, and some are under-utilised.
Despite these developments, there remain challenges around the health information system and quality services delivery in Bhutanese hospitals and clinics. These include a paper-based approach, the lack of patient-based data platform, poor medical data, poor patient follow-up practices and poor treatment outcomes, healthcare professionals resisting change, same data being collected repetitively and many health facilities without connectivity (Internet), with low patient engagement.
There are no standards in terms of data or systems, leading to poor reporting, late decisions, poor planning, and huge healthcare expenditure, resulting in inefficiencies and ineffectiveness in the delivery of healthcare to the people. Bhutan recorded one million lab tests in 2018,4 which is alarming for a population of just 0.7 million. As in many countries, telemedicine programmes suffered the most.
This explains His Majesty the King’s initiatives to improve the national healthcare service, and encourage Bhutanese to adopt technology to improve service delivery. The 71st World Health Assembly Resolution,5 the ICM Act 2018, the commitment of current government and partners, readiness of health facilities, and National eHealth Strategy 2018 are the main drivers behind the ministry’s approach to digital solutions.
The ministry’s attempt to develop an ICT Masterplan for the health sector in 2015 did not succeed so, in 2017, the ICT Division was established in the ministry to spearhead all the ICT/ehealth activities and guide the programmes. Prior to this, ICT professionals were scattered among the programmes and were unaware of all the common ICT related issues, and their efforts and competency were not used optimally. This was followed by the development of the National eHealth Strategy and Work Plan, which served as a lighthouse for ICT initiatives in the ministry.
This also established the National eHealth Steering Committee, which served as the governing body for any ICT activities for the ministry, and the eHeatlh Technical Working Group was established to carry out review or carry out the ICT activities.
The project known as the Electronic Patient Information System (ePIS) is an attempt to roll out hospital information systems for the health sector across Bhutan, which is expected to function like Enterprise Resource Planning (ERP) System of companies, where patients’ records could be accessed by patients and authorised professionals from anywhere with network health facilities. The project was mainly supported through an ADB grant, while the World Health Organisation and the Royal Government of Bhutan also made contributions.
This project is a component of Digital Drukyul (National IT) Flagship Programme, the national priority project of the new government reporting to the Prime Minister through the Department of Information Technology and Telecommunications (DITT) and Gross National Happiness Commission (GNHC). In the Ministry of Health, the eHealth Steering Committee governs the project, while eHealth Technical Working Group carries out the technical work related to the project, as established through the National eHealth Strategy.
The health sector had tried to implement similar projects in the past but was not successful. The current project made an assessment as to why it failed previously to mitigate similar challenges, and to ensure the success of the project this time.
Such ICT projects in hospitals are very complex in nature, as it deals with human lives and, therefore, requires high health standards (such as HL7, DICOM, ICD11, SNOMED) in order to integrate with medical devices. The features required in the system are mainly to digitise and improve functionalities and processes of the hospital, and share data for analytics, which could be used for timely decision-making by health professionals and focused planning by bureaucrats to save lives and cut down the huge healthcare expenditure the government is incurring currently.
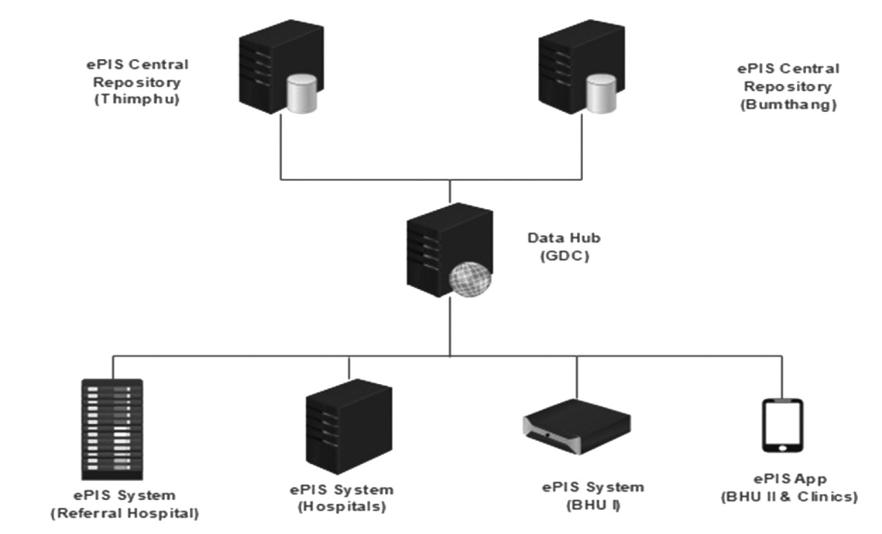
The “Whole of Government” ICT solutions, such as digital identity and data hub, are to be used, or provisions to be kept. To ensure no data collection is duplicated, all the existing systems and new systems will be interconnected, and data shall be exchanged via health data hub. The solution is to be rolled out in all the 300 or so health facilities in the country, and also in the ministry and other allied health institutions (Medical University, Health Council, Narcotics Agency, Drug Regulatory Authority etc.) with hospital premise deployment architecture, with a central repository in Government Data Centre (GDC) in Thimphu and apps for both health professionals and patients. The proposed timeline of the project included the signing of the contract by April 2020, starting the rollout in the Jigme Dorji Wangchuck National Referral Hospital ( JDWNRH) by June 2020, and the project to end in December 2022.
Some of the previous constraints — such as poor coordination, resistance from users, poor ICT support, poor network, and vendor locked system — are overcome currently through various means. Connectivity and digital literacy have been highlighted in the health bill as a prerequisite to introduction of solutions, and use of technology has been made a priority, and mandatory.
One of the stakeholders of the project includes DITT, which ensures the project has adequate manpower, health professionals are digitally literate, and all health facilities are interconnected. The assessment by project shows that more than 80 percent of facilities have connectivity compared and the new generation of health professionals is more receptive to introduction to such an initiative, as many of them have been wasting time collecting and sending similar reports to various programmes, instead of providing service to patients.
The Annual Info Comm Bulletin of the Ministry of Information and Communications6 also shows that mobile penetration has reached 95.8 percent of the population. To ensure that local ICT competency is built, the government has directed a project (of developing the solution) to be carried out by an ICT Company under Druk Holding and Investments, so that Bhutan does not have to depend on external firms or individuals for ICT support, which is often time consuming and challenging. The national health Enterprise Architecture Blueprint is currently under process to help Bhutan to realise these goals, and also define all the missing standards.
The current government’s party manifesto7 states:
“We will establish and implement an online patient record system, following which the responsibility of looking after and following up on patients’ health will be with the hospitals. We will build a system that enables the hospital to track a patient’s health and ensure they receive timely medications, especially for those on long-term treatment, at a place convenient to them.”
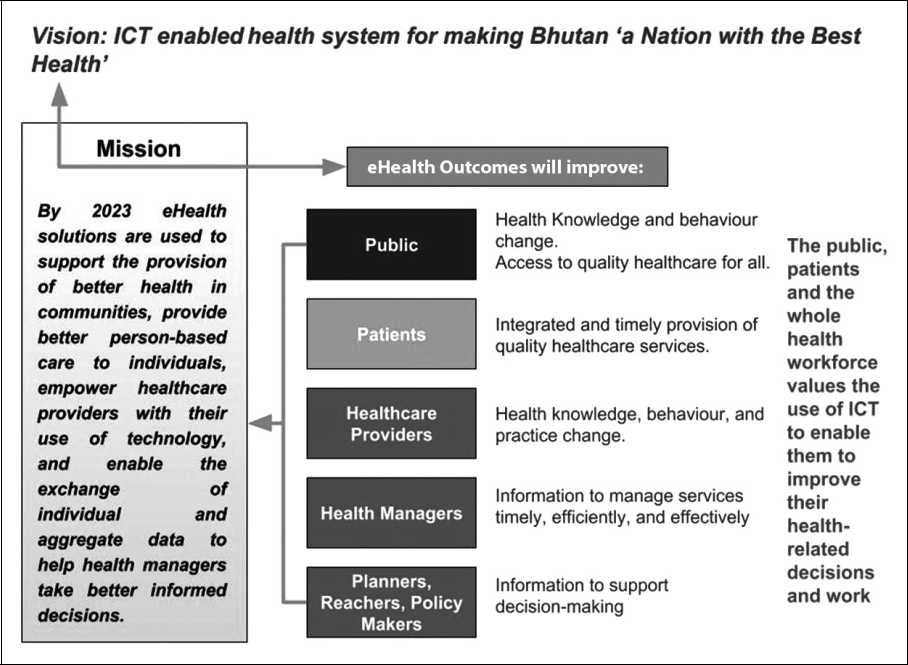
It ensures the commitment by endorsing the project as a priority project, as stated in the Prime Minister’s State of Nation Address 2019.8 As reflected in the vision of the National eHealth Strategy, which promises on “ICT enabled health system for making Bhutan a nation with the best health”, along with the mission for solutions to be used to support the provision of better person- based healthcare to individuals, empower healthcare providers with use of technology, and enable the exchange of individual and aggregated data to help health managers make better decisions by 2023. This is expected to improve health knowledge and behaviour change of the public, access to quality healthcare for all, and provide integrated and timely provision of service to patients.
Besides rolling out integrated software across all the health facilities, the project is also planning to use remote telemedicine solutions to reach the unreached through apps for health professionals. The public can also be a part of the solution by using the apps provided to them, in carrying out registrations and checking appointments. Artificial Intelligence in the system will be used to remind the public about upcoming appointments, while clinicians will be notified of wrong medications and disease outbreaks.
While there are many risks, as stated in the Transforming health care through Bhutan’s digital health strategy (2019), such a system will not only make health care services better but also address Bhutan’s manpower shortage.
Therefore, it is imperative for Bhutan to adopt such a system by any means; it will be expensive in the beginning, but will soon pay off in terms of efficiency and huge healthcare expenditure savings. If Bhutan can roll out this project successfully, Bhutan will be one among a few countries in the world to roll out standardised integrated healthcare ICT solutions across the nation, including non-allopathic facilities (Traditional Medicine Hospital/Clinics). This will help Bhutan achieve the goal of Universal Health Coverage (UHC), towards which every nation in the world is aspiring.
References
1 His Majesty The King Jigme K. N. Wangchuck’s Address at the 14th RUB Convocation - 24 May 2019.Retrieved from http://www.rub.edu.bt/index.php/en/the-university/chancellor1/588-his-majesty-the-king-s-address-at-the-14th-rub-convocation-24-may-2019
2 Annual Health Bulletin 2019, Ministry of Health, Royal Government of Bhutan
3 National Health Policy of Bhutan 2011. (n.d.). Retrieved March 2, 2020, from http://apps.who.int/ medicinedocs/en/d/Js19416en/
4 Annual Health Bulletin 2018
5 The 71st World Health Assembly Resolution. (n.d.). Retrieved March 2, 2020, from http://apps.who.int/ gb/e/e_wha71.html
6 10th Annual Info Comm and Transport Statistical Bulletin 2019. (2020, February 6). Retrieved March 3, 2020, from https://www.moic.gov.bt/wp-content/uploads/2019/03/10th-Annual-Info-Comm-and-Transport-Statistical-Bulletin-2019.pdf
7 Narrowing the gap (n.d.). Retrieved March 2, 2020, from https://www.ecb.bt/pp/dnt/dntmanifesto2018. pdf
8 State of Nation 2019. Retrieved March 2, 2020, from https://www.cabinet.gov.bt/wp-content/ uploads/2019/07/State-of-Nation-for-web.pdf